Declaring a “major incident” may seem like an extreme option to protect our health and social care services.
While talk is currently dominated by lifting restrictions, in Hull and the East Riding we seem to be struggling.
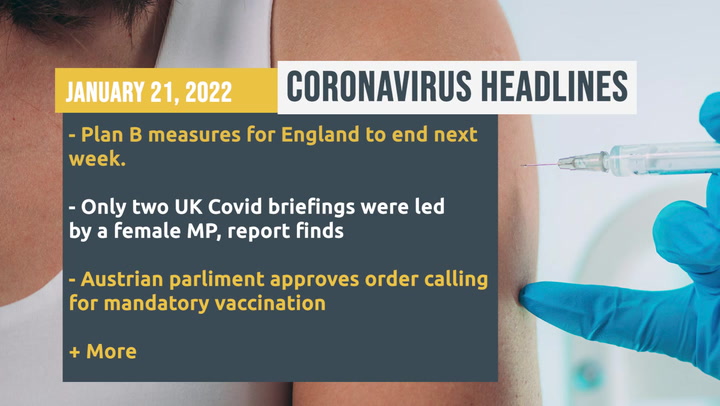
For the latest coronavius news click here.
But this is a complex situation and, while it would be harsh to call the system a house of cards, issues in one area can have a knock on effect elsewhere.
For instance, staff issues may prevent care homes from taking back residents who have been in hospital which means they have to remain in the ward which create a further strain on the doctors and nurses.
So just what is going on in Hull’s NHS right now?
(Image: Katie Pugh)
Staff sickness
Hull University Teaching Hospitals NHS Trust, which runs Hull Royal Infirmary and Castle Hill Hospital, is feeling the pressure on a number of sides.
Hull Live understands seven per cent of the workforce is off sick which is two per cent more than normal and considerably higher than the national average of two per cent.
And while that two per cent might not seem like much it does represent 200 more people off.
Making it worse is the fact a high proportion of these absences are frontline staff – such as doctors and nurses – rather than admin or backroom staff.
When you take into account the fact they cannot move patients back to care homes because those homes are also struggling with a lack of staff, then you begin to see why such action was necessary.
Hospitals are already still trying to deal with the backlog of other operations and procedures cancelled during previous waves of the pandemic.
This declaration seems to go against the grain and many maybe puzzled when Covid cases seem to be falling rapidly.
But there are a number of factors at play.
Video Unavailable
Huge rise in Covid cases
Firstly, while cases are falling, they are doing so from a very high level.
While the Omicron variant is not as deadly as previous ones, it is far more transmissible which has had a huge rise in cases..
Previous lockdowns have been prompted by a weekly Covid rate of just a few hundred cases per week but some areas of East Yorkshire have seen rates top 3,000 and the weekly average in Hull and the East Riding has been well over 1,000 for the past month.
The R rate – the reproduction number – is the average number of secondary infections produced by a single infected person.
An R value of 1 means that on average every person who is infected will infect 1 other person.

(Image: Katie Pugh)
But since December, that number has been above one which means the virus is spreading. So, while cases might be falling, the rate remains very high.
Hull still has a rate of 1,157 while in the East Riding it stands at 987.
For context, in October 2020 when Hull had by far the highest rate in the country the rate was only around 740.
Secondly, there is always a lag between the rise in cases and the impact on hospitalisations and deaths.
It would have been a couple of weeks ago when cases in our area were at their highest and now we are seeing Covid patients continuing to rise in our area.
Not long ago the patient numbers were steady at around the 40-60 mark but now that number is approached 130 earlier this week but has now dropped again to 117.
Thankfully, the number of Covid patients in intensive care remains relatively low with just three at the last count.
Deaths have also remained lower than in previous waves. There have been 21 deaths recorded in January so far but that rate is far below the total for January last year when there were 187 deaths.
Behind the curve
Thirdly, Hull always seems to be behind the curve.
Cases remained relatively low in the area at a time when cases were out of control in London around Christmas time.
When cases began plummeting in London cases were still rising here.
Can’t see this survey? Click here
More widely, there are concerns the NHS has been underfunded and staff have been stretched after an exhausting couple of years.
Hull West and Hessle MP Emma Hardy said on Twitter: “It’s no surprise that staff are exhausted after working so hard on the front line of the pandemic for two years. A pay rise is the least they deserve.
“The Government must make sure that we never again face a pandemic with an NHS so understaffed and under resourced.”
The rather London-centric Government has now been prompted to ease restrictions despite cases remaining high in the north.
The major incident announcement should not worry us unduly but it should act as a warning that this pandemic is far from over despite people retuning to offices and masks being ditched.
For most of us, a major incident involves some horrendous natural disaster or a terrorist attack.
But sometimes the threat to the public can be a little more subtle – such as a strain being placed on our health services.
Major incidents are declared by the Local Resilience Forum (LFR), which comprises managers from the emergency services, local authorities, the NHS and others.
By declaring a major incident, it enables local leaders – usually from councils, police, the health and fire services – to request extra support from the government and to better coordinate action between emergency services.
The effect on patients
But it might also involve prioritising resources in services.
In hospitals that could mean cancelling planned surgery; discharging medically-fit patients; moving staff, including managers, to other duties; preparing in detail for extra, urgent workloads and making more use of volunteer help.
In social care, councils may ask family members to pitch in and look after relatives and they may be compensated if they have to take unpaid leave to do so.

Care homes are jot only being effected by absences from the recent Omicron wave but they have lost staff over the last two years.
Care home workers have found the job very tough and do not feel they have always had the support they need, particularly early on, which has led to a drain in staff numbers generally.
Major incidents have previously been declared in the UK for terror attacks, floods, infernos, street stabbings and gas leaks, including the Grenfell Tower fire in 2017 and the terror attacks at Westminster Bridge and London Bridge.
Hospitals and health trusts have also done so during the Covid-19 pandemic in areas like London and Manchester.
Major incidents are declared at the discretion of local services to manage emergencies
They are defined as beyond the scope of business-as-usual operations, and is likely to involve serious harm, damage, disruption or risk to human life or welfare, essential services, the environment or national security”.
The declaration also allows scope for different services and organisations to pull together and carry out different duties.
Chief fire officer Chris Blacksell and Humber LRF chairman said yesterday: “Declaring a major incident enables the agencies to come together to step up planning and the response to manage these increased pressures on local health and care services and helps us to work together more effectively across multiple organisations.
“We have implemented a number of measures to try and alleviate some of the pressures for example Humberside Fire and Rescue Service is expanding the medical response we already provide to older people who fall in their own home in Hull, more widely across the rest of the Humber area.”
The main aim of declaring a major incident is to protect the most vulnerable and ensure they are well looked after.
Once staff begin returning and some kind of normality resumes, the major incident will end.
To sign up for the Hull Live newsletter,click here.

